Let's reinventMedicaid together.
We're building the technology to serve millions of Americans with the same usability and intelligence you'd expect from leading technology companies. Our AI instantly spots fraud patterns humans miss, citizens enroll in minutes instead of months, and every interaction is as simple as ordering from Amazon. Applications arrive complete and accurate, dramatically reducing follow-up calls and staff time spent correcting errors. Finally, Medicaid that actually works.
$68B
Annual Medicaid Fraud
28M
Eligible but Not Enrolled
47%
Audit Failure Rate

91M
Americans Covered
50%
Cost Reduction
98%
Accuracy Rate
California Medicaid Analytics
Eligible Population
5.2M
Coverage Rate
78%
Coverage Gaps
1.1M
Fraud Detected
$890M
Potential Annual Savings
$2.3B
78% improvement over current system
Fraud Blocked!
$2.3M saved
No MoreGarbage In, Garbage Out
Every smartphone has bank-level biometric security built in. We use Face ID and voice recognition to verify identity instantly – no more fake applications, no more identity theft, no more fraud slipping through.
Biometric Verification
Face ID and voice match ensure the right person gets benefits
Document Matching
AI compares driver's licenses to applications in real-time
Fraud Pattern Detection
AI spots fraudulent documents before they're even submitted
Snap & Submit
Citizens photograph documents – we verify authenticity instantly
$68 Billion Lost to Fraud Annually
Traditional paper-based verification fails. Our AI catches fraud patterns that humans miss, saving billions while ensuring legitimate beneficiaries get instant access to care.
Verifying Identity
Look at your camera
Identity Verified
No Fake IDs
Bank-Level Security
Virtual Case Worker
Processes applications, verifies eligibility, and guides citizens through enrollment
Fraud Detector
Identifies patterns, blocks fraudulent claims, and protects program integrity
Presumptive Analyzer
Fast-tracks emergency coverage for pregnant women and children
Application Processor
Handles renewals, updates, and document collection in 75+ languages
1000x Your WorkforceWith Agentic AI
Specialized AI agents orchestrate every aspect of Medicaid processing – from eligibility screening to fraud detection. They collaborate in real-time, handling millions of cases simultaneously in 75+ languages.
- 90% reduction in processing time – AI handles everything from intake to approval
- $12,000 saved per employee annually – automation eliminates repetitive tasks
- Zero backlogs – applications process instantly, 24/7/365
- Proactive outreach – AI finds and contacts eligible citizens automatically

HELLO
I AM...
Covered
HIPAA Compliant
Coverage Activated
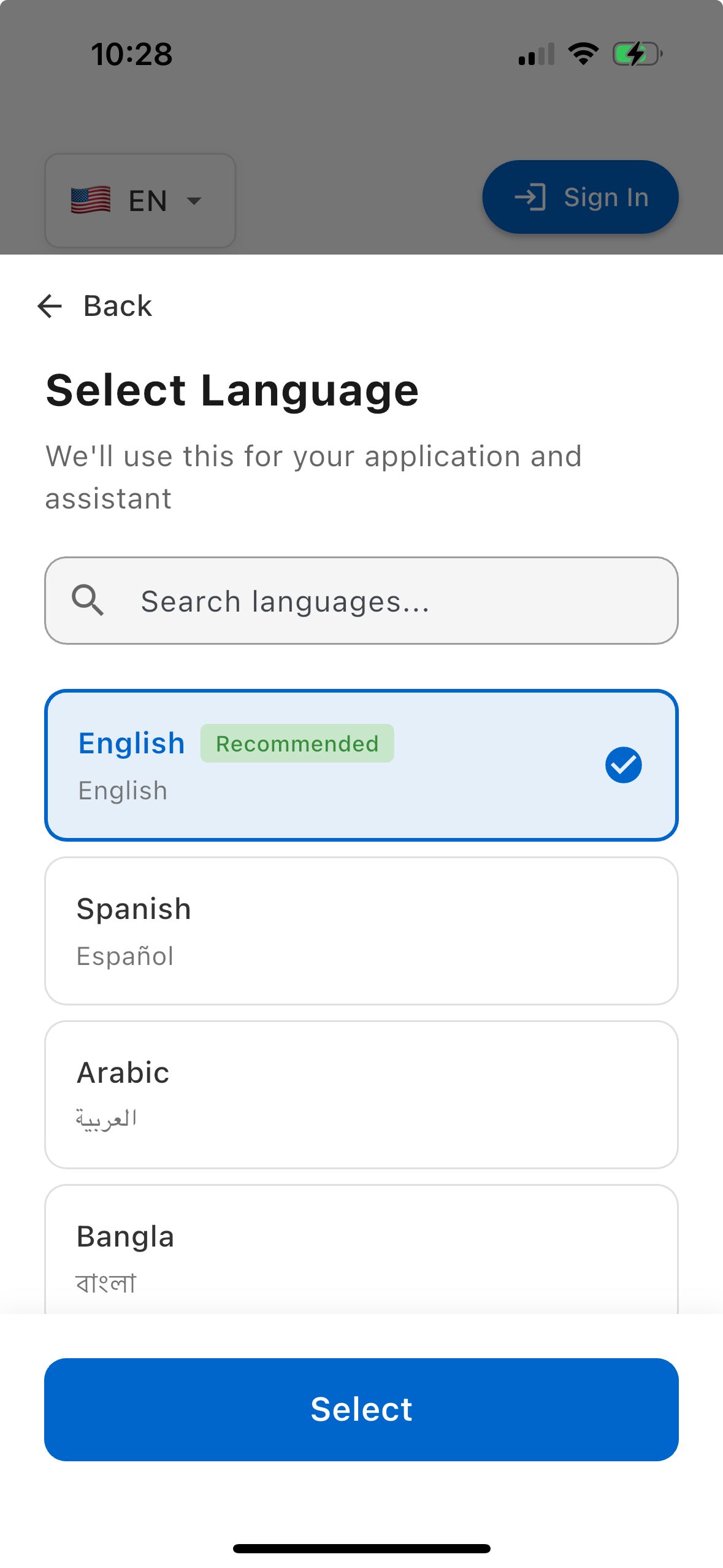
A Mobile App to ServeYour Medicaid Population
Nearly every Medicaid recipient has a phone. Our app reaches them where they are, in their language, with ease and security. Built-in biometric security keeps fraudsters out while making it simple for legitimate beneficiaries.
75+ Languages
Voice-guided in every language your citizens speak
Biometric Security
Face ID and voice recognition prevent fraud
Built with Dignity
Beautiful, respectful interface they can be proud of
Voice First
No typing required - just speak naturally
Security That Works for Everyone
The phone's built-in biometric technology verifies identity instantly. No passwords to remember. No documents to upload. Just their face or voice.
AI That Speaks Your Language.Real Conversations. Real Results.
Stop Making People Wait in Line
Your citizens are already on their phones. Meet them there with AI that actually understands them - in their language, on their schedule. No more 3-hour waits. No more paper forms. Just real help when they need it.
- 75+ Languages: AI assistants speak every language in your state
- Omnichannel Access: Phone, SMS, web, mobile, and in-person kiosks
- Document Automation: OCR and auto-fill reduce application time by 80%
- Proactive Outreach: AI identifies and contacts eligible but unenrolled citizens
✓ Real-time AI in 75+ Languages
75+
Languages
Nov 2025
Launch Date
Built Security-FirstFrom Day One
We're new, but security and privacy aren't an afterthought—they're our foundation. All government certifications currently in process. Join our community to stay updated.
FedRAMP High
Highest authorization level
StateRAMP
State security certified
NIST 800-53
Full compliance
AWS GovCloud
Sovereign infrastructure
GOVERNMENT PILOT PROGRAM
Experience the Future ofState Medicaid Services
See how HeyMedicaid handles real constituent calls in 75+ languages.
Watch fraud detection and compliance in action.
State Impact
Coverage Gaps
-67%
Fraud Detection
+94%
Processing Time
-85%
Live Constituent Line
Sample Medicaid Application: Nebraska
Available in all 50 states
FedRAMP certified • HIPAA compliant
Compliance
CMS certified
MAGI compliant
Real-time reporting
Join Leading States in
Medicaid Modernization
Reduce fraud by 40%, improve coverage rates by 25%, and ensure 100% CMS compliance. Schedule a confidential briefing today.